Can I Use CBD With Chemotherapy? (UK 2026 Guide)
In this guide, I will walk you through the practical, UK-relevant way to think about CBD during chemotherapy. You will learn what to ask your oncology team, what interactions are theoretically possible, how to approach timing and dose if you are given the green light, and how to choose a product with confidence and clear lab testing.
Why chemotherapy changes the CBD conversation
When you are on chemotherapy, your body is often under extra strain. You might be dealing with appetite changes, nausea, fatigue, sleep disruption, mood changes, and the mental load of appointments and blood tests.
It makes total sense to look for gentle, everyday tools that help you feel a bit more like yourself. Some people report that CBD supports relaxation, helps them feel more settled, or fits into a calming evening routine. But chemo is not the same as “everyday life”, and the margin for error is smaller.
Consider this: your oncology team has chosen your medication and dose based on how it is absorbed, broken down, and cleared from your body. Adding anything new, including CBD, can potentially change that picture. So the right mindset is not “Can CBD help?” It is “Can CBD be used safely alongside my exact treatment plan?”
If you want to brush up on CBD basics first, read our parent guide on CBD Oil.
How CBD could interact with chemo and other medicines
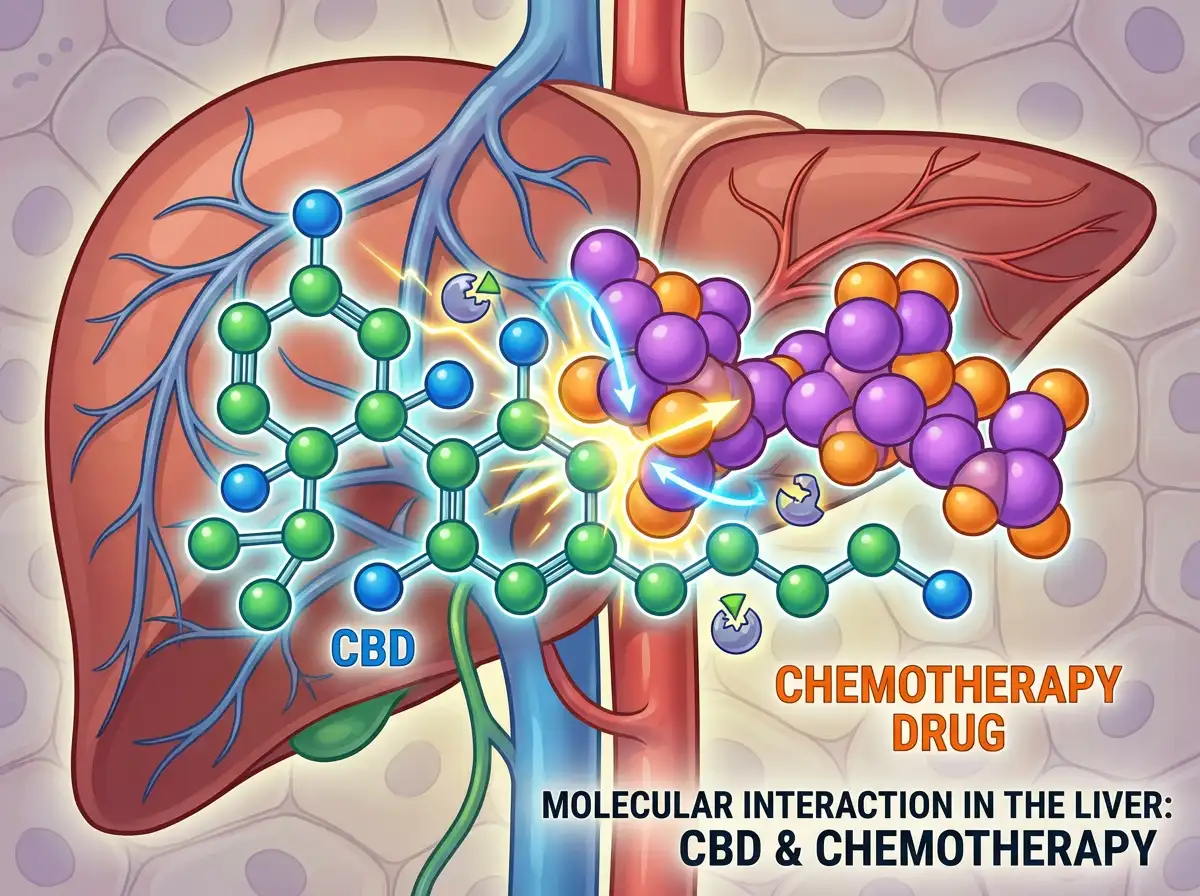
1) The main issue is metabolism (how your liver processes medicines)
CBD is processed in the body using enzyme pathways in the liver. Some chemotherapy medicines, anti-sickness tablets, steroids, pain relief, and anxiety or sleep medicines also use overlapping pathways.
In practice, this means CBD could affect the level of another medicine in your blood, either raising it (more side effects risk) or lowering it (less effect). Whether that happens depends on the drug, your dose, your genetics, your liver function, and what else you are taking.
Because chemo regimens differ so much, there is no one universal “safe combo” list that covers everyone. This is why the next section, what to ask your team, matters.
2) Side effects can overlap
Even when there is no clear interaction, CBD can cause side effects in some people, especially at higher doses. The common ones reported include sleepiness, light-headedness, dry mouth, and digestive upset.
Now, when it comes to chemotherapy, you might already be managing fatigue, constipation or diarrhoea, appetite changes, and nausea. Stacking anything that could worsen those symptoms is not ideal, even if it is “only a supplement”.
3) Immunity, infection risk, and “unknown unknowns”
During chemo, your immune system can be suppressed. That makes product quality and contamination risk more relevant than ever. With CBD, the big concerns are inaccurate labels, poor-quality extracts, or contaminants like residual solvents, heavy metals, or pesticides if a brand does not test properly.
Research into CBD alongside cancer treatment is still evolving. So we have to be honest: there are limits to what anyone can say with certainty. Your medical team is the final decision-maker here.
For a broader look at interactions beyond chemo, this article helps: CBD and Medication.
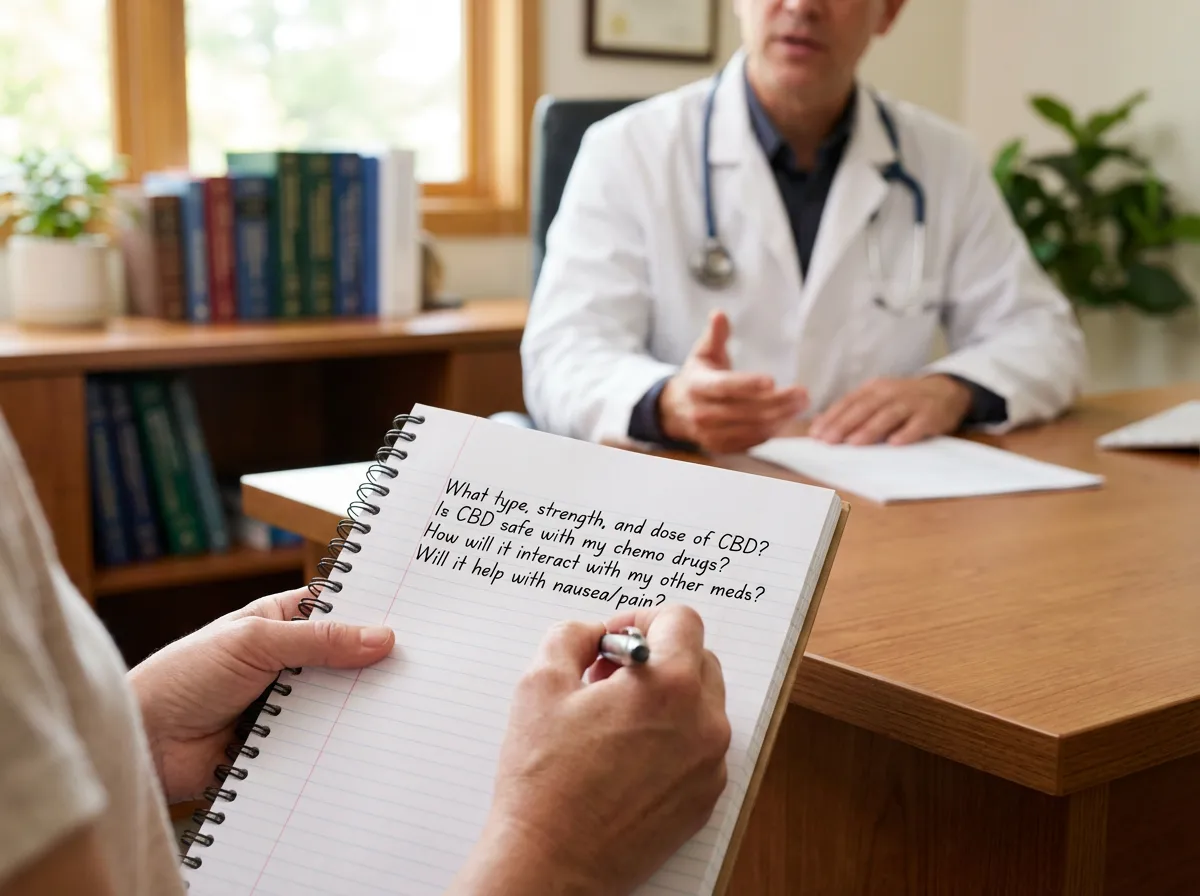
What to ask your oncology team (and why it matters)
What many people overlook is that “I’m taking CBD” is not a single, clear statement. Your team needs specifics: what type, what strength, what dose, how often, and how you take it.
Take this list to your next appointment or chemo unit call:
- Tell them your full medication list, including anti-sickness tablets, pain relief, sleeping tablets, antidepressants, and herbal supplements.
- Ask: “Are any of my chemo drugs or support meds likely to interact with CBD through liver enzymes?”
- Ask: “If I did try CBD, is there a preferred timing window away from my chemo days or oral chemo dose?”
- Ask: “Are there reasons to avoid full spectrum products because of trace THC?”
- Ask: “Would you prefer I avoid CBD completely during this cycle, and revisit later?”
Think of it this way: your team is not judging you for asking. They are managing risk. The clearer you are, the easier it is for them to advise you sensibly.
If you get a “yes”: safer ways to start (dose, timing, tracking)
If your oncology team is comfortable with you trying CBD, keep it boring and consistent. Chemo is not the time for experimenting with huge doses, mixing multiple products, or changing three things at once.
Start low, go slow, stay consistent
Most people do best starting with a small dose, taken at the same time each day, then slowly adjusting. The UK Food Standards Agency recommends healthy adults do not exceed 70mg CBD per day. During chemotherapy, your clinician may want you well below that, or to avoid CBD altogether.
From a practical standpoint, keep a simple log for 7 to 14 days. Note your CBD dose, the time you took it, and anything you notice such as sleepiness, appetite changes, nausea, or tummy upset. If something shifts, you and your team have useful information rather than guesswork.
If you want help estimating a starting point, our CBD Dosage Calculator can give a general guide, but it does not replace oncology advice.
Timing: keep separation where possible
If you are taking oral chemotherapy or time-critical medicines, your team may suggest spacing CBD away from doses. That is a sensible approach in many supplement conversations, but do not self-prescribe a schedule. Ask for a plan that fits your regimen.
Avoid stacking sedatives
If you are already on medications that make you drowsy, adding CBD can sometimes tip you into feeling wiped out. If you do try it, many people prefer evening use for this reason, but again, check with your clinician.
CBD formats explained: oils, water soluble, and patches
When you are dealing with chemo side effects, the “best” format is often the one you can actually tolerate consistently. Taste changes, nausea, and swallowing difficulties can make certain products a no-go.
CBD oil drops (sublingual)
CBD oils are usually taken under the tongue for a short hold before swallowing. This can suit people who like precise drop-by-drop control. One example is a full spectrum oil like 10% CBD Oil [1000mg CBD] (CBD One Signature Blend No.2), which is taken as drops under the tongue.
Oils do have a natural hemp taste, which some people love and others struggle with, especially during treatment. If taste is an issue, do not force it. Consistency matters more than willpower.
Water soluble CBD (mix into a drink)
Water soluble CBD is designed to mix into hot or cold drinks. Some people find this easier during periods of nausea, because it feels more like a normal part of a morning routine. CBD One’s Absorb range, for example, uses a pump format that you add to a drink, then adjust gradually.
If you want to browse formats, you can explore the Water Soluble CBD category. It is a useful option if oils are too strong-tasting for you.
CBD patches (transdermal)
Patches are applied to the skin and release CBD slowly. They also give you a measured amount per patch, which some people find reassuring when they want consistency. CBD One patches are CBD isolate (THC-free) and designed for slow release.
Now, when it comes to chemotherapy, always check skin sensitivity. Chemo and steroids can make skin more reactive, and adhesives may irritate. If you are considering patches, patch-test first and stop if you get redness or itching.
If you are weighing up options, our CBD Product Comparison guide can help you think through oils vs water soluble vs patches in a structured way.
Quality and label checks that matter more during chemo
The reality is that product quality is not a “nice to have” when your body is under pressure. It is a safety issue.
Use this checklist before you buy anything:
- Look for recent third-party lab reports (COAs) for cannabinoids and contaminants.
- Check the CBD amount per dose, not just “total mg per bottle”.
- Know the spectrum: full spectrum contains multiple cannabinoids and terpenes plus trace THC within legal limits; isolate is THC-free.
- Avoid products making medical claims about cancer, chemo, or tumour reduction. In the UK, CBD is not a medicine and cannot be marketed as one.
- Keep ingredients simple. Flavourings, sweeteners, or extra botanicals can be harder to tolerate during treatment.
At CBD One, we are big on full spectrum extracts for the Entourage Effect in our core oils and water soluble range, and we publish lab verification so you can see what is in the bottle. But during chemotherapy, the key point is this: choose any brand that can show transparent testing and does not overpromise.
If you are browsing, the CBD Oils category is a good place to compare strengths and serving styles without getting lost.
For a wider safety overview, this is worth a read: Is CBD Oil Safe?
CBD and immunotherapy: what changes, what stays the same
A question that comes up a lot now is not just chemotherapy, but immunotherapy too. If you are on an immune-based treatment, the same basic principle applies: do not assume CBD is automatically fine just because it is widely sold.
Here’s the thing: the “risk” conversation tends to come back to two areas, interaction potential and side effects. Immunotherapy protocols can be very different from chemo, and people can be on combinations, so your team’s advice has to be specific to you.
From a practical standpoint, if you are on immunotherapy (or chemo plus immunotherapy), it helps to ask one extra question: “Are you concerned about CBD affecting how my treatment works, or are you mainly concerned about side effects and metabolism?” That gives your clinician room to explain their thinking, and it gives you clearer boundaries about what is and is not OK to trial.
And just to keep it grounded: even if your team is comfortable with CBD, they may still want you to avoid it around infusion days, avoid higher doses, or avoid certain product types. That is not them being awkward, it is them trying to reduce variables.
A practical interaction check: medicines often used alongside chemo
People often focus on the chemotherapy drug itself, but in real life you are usually given a “supporting cast” of medicines. That is where the interaction conversation gets more relevant, because you might be taking several things that already affect sleep, digestion, or dizziness.
Consider this quick checklist and use it to guide your conversation with your team or pharmacist. It is not a list of “do not combine”, it is a reminder of what to mention:
- Anti-sickness medicines, especially if they already make you drowsy or constipated.
- Steroids, which can affect sleep and mood and can make it harder to work out what is causing what.
- Opioid pain relief, which can add sedation and constipation risk.
- Sleeping tablets or anti-anxiety medicines, which may stack with CBD’s calming effects for some people.
- Antidepressants (including SSRIs), because some are metabolised through overlapping liver pathways.
- Blood thinners or medicines where small level changes matter, because your team may prefer to minimise variables.
What many people overlook is how useful one simple sentence can be: “If I try CBD, what side effects would you want me to watch for that would mean I should stop?” That turns the discussion into a safety plan, not a debate.
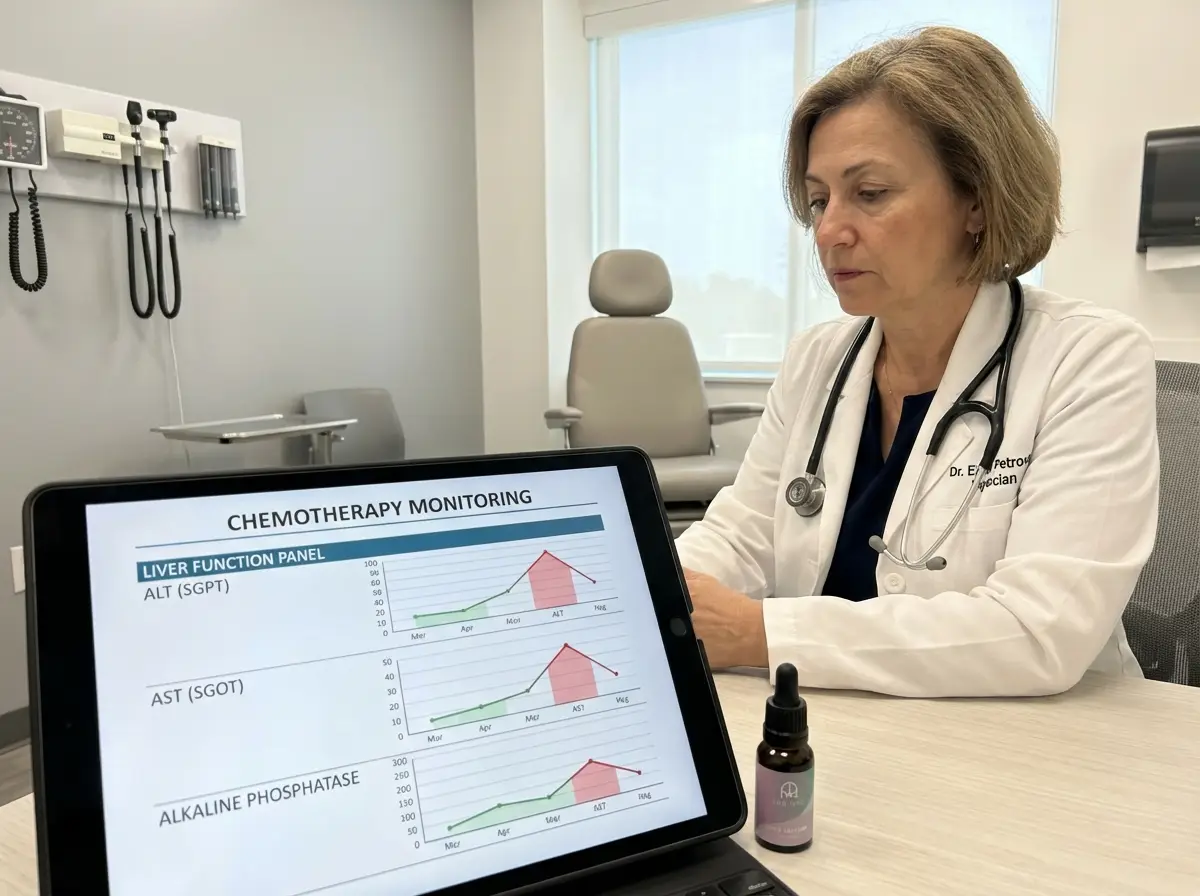
CBD and liver blood tests: why your team may monitor more closely
If you are on chemotherapy, you will be very familiar with blood tests. Liver markers are often part of that monitoring because your liver plays a big role in processing medicines, and treatment itself can affect liver function.
CBD is also processed in the liver. Some people worry that this automatically means “CBD damages the liver”, but the more accurate way to think about it is: liver processing is one reason your team may be more cautious with supplements, particularly at higher doses or when multiple medicines are involved.
The practical takeaway is simple. If your team agrees you can trial CBD, tell them if you change the dose later, and keep an eye on any advice linked to your blood results. If your clinician flags liver test changes, or asks you to pause supplements, it is sensible to follow that and reassess when you are stable.
If taste, nausea, or swallowing are issues: making CBD more tolerable
Chemo can change your relationship with food and drink in a way that is hard to explain unless you have lived it. Taste can feel “off”, smells can trigger nausea, and even swallowing can become a bit of a hurdle on rough days.
If CBD is approved for you, the goal is not to power through. It is to make it easy enough that you can be consistent without adding stress. A few practical ideas that many people find helpful:
- If oils make you gag, do not force it. A different format may be easier to stick with.
- If you use water soluble CBD, start with a small amount in a familiar drink that you already tolerate. Keep the rest of your routine the same so you can spot changes.
- If your mouth is dry or sensitive, avoid adding CBD into very acidic drinks. Choose something gentle that does not irritate.
- If patches appeal because you cannot face swallowing anything, remember skin can be reactive during treatment. Patch-test first and rotate application sites.
Think of it this way: the “right” CBD plan during chemo is the one that fits around your hard days, not your good days.
When to avoid CBD or stop and get advice
Sometimes the safest choice is a clear “not right now”. If your oncology team advises against CBD, follow that guidance and revisit later if appropriate.
Stop and seek medical advice if you notice new or worsening side effects after starting CBD, especially unusual sleepiness, dizziness, ongoing diarrhoea, vomiting, or anything that affects your ability to eat, drink, or take your prescribed medicines.
Also be cautious if you have known liver issues, are on multiple medications, or your blood tests show changes that your team is monitoring closely. Chemo is very individual, and so is your risk profile.
Finally, if you are using CBD to cope emotionally, I completely understand that instinct. Just make sure you also ask your team about proper support options such as counselling, Macmillan resources, or medication reviews. CBD can be part of a wellness routine for some people, but it should not be your only support.
Frequently Asked Questions
Can I use CBD with chemotherapy?
Possibly, but you should only do it with your oncology team’s awareness and approval. The main concern is potential interaction with how certain medicines are metabolised, plus overlapping side effects like fatigue or digestive upset. Chemo regimens vary hugely, so what is fine for one person may not be for another. If your team says it is acceptable, start with a low dose, keep it consistent, and track how you feel. If anything changes, stop and ask for advice rather than pushing through.
Can CBD replace anti-sickness medication during chemo?
No. In the UK, over-the-counter CBD products are not medicines and should not replace prescribed or recommended anti-sickness medication. Some people report CBD feels calming, which may indirectly help them cope with discomfort, but that is different from treating nausea or preventing vomiting. If nausea is not controlled, speak to your chemo team quickly because there are multiple anti-emetic options and dosing approaches. If you want to trial CBD alongside, that should be a clinician-led decision with clear boundaries.
Can CBD help with nausea?
Some users report CBD feels settling, especially when anxiety is part of the nausea picture. That said, nausea has many causes, and during chemotherapy it can be directly medication-related. Research is still developing and you should not assume CBD will help or that it is risk-free in this context. If you do get clinician approval, consider a form you can tolerate on rough days, and keep the dose low. If nausea persists or you cannot keep fluids down, treat that as urgent and contact your chemo unit.
Is full spectrum CBD safe during chemotherapy?
Full spectrum CBD contains CBD plus other naturally occurring hemp compounds, including trace THC within UK legal limits. Some clinicians prefer patients avoid THC entirely during treatment, even at trace levels, while others focus mainly on interaction risk and product quality. This is why you should share the exact product type with your team. If they advise avoiding THC, an isolate product may be more appropriate. Whatever you choose, prioritise third-party lab reports and avoid products making medical claims.
Are CBD patches safer than CBD oil during chemo?
Not automatically. Patches can offer measured dosing and slow release, which some people prefer for consistency. But chemotherapy can make skin more sensitive, and adhesives can irritate or cause redness. Also, “safer” really depends on interaction potential with your medicines, which is not purely about format. If your team approves CBD generally, a patch may be an option, but patch-test first and stop if you get irritation. If you are using dressings, PICC lines, or sensitive areas, ask a nurse where not to place one.
What CBD dose is considered safe in the UK?
The UK Food Standards Agency advises healthy adults not to exceed 70mg of CBD per day. That is a general public guideline, not a chemotherapy-specific recommendation. During chemo, a clinician may advise a much lower dose, or none at all, depending on your treatment and other medicines. If you are approved to try CBD, start low and increase slowly only if needed. Tools like a CBD Dosage Calculator can provide general guidance, but your oncology team’s advice comes first.
Can you use CBD oil with sertraline?
Sertraline is an SSRI, and CBD may affect liver enzyme pathways that also process some antidepressants. That does not mean the combination is always unsafe, but it does mean you should be cautious and speak to your prescriber or pharmacist before combining them. Watch for increased drowsiness, dizziness, or changes in how you feel emotionally, and do not change your prescribed dose without medical support. If you are also on chemotherapy, the “check first” advice becomes even more important.
Can you use CBD patches with sertraline?
Even though patches avoid the digestive system, CBD still enters the body and could, in theory, contribute to interactions or side effects like sleepiness. Some people like patches because the dose per patch is clear and the release is slow. But if you take sertraline, speak to a pharmacist or prescriber before adding CBD in any format. Also consider skin sensitivity if you are under medical stress or on treatments that affect the skin. If you do trial it, keep everything else stable so you can spot changes.
Can CBD oil help with menopause or perimenopause if I am also having chemo?
Some people look to CBD for sleep, stress, and general wellbeing during perimenopause or menopause, and chemo can add another layer of hormonal disruption depending on your treatment. The key is not to self-diagnose what is causing symptoms like night sweats, anxiety, or poor sleep. Speak to your oncology team and GP, as there may be treatment-related reasons and safer supportive options. If CBD is approved, treat it as a gentle wellness tool, not a solution, and keep dose and timing consistent.
How do I choose a CBD product if my oncology team says it is OK?
Keep it simple and transparent. Choose a product with third-party lab reports, clear CBD per dose, and minimal ingredients. Decide on spectrum based on your team’s preference, full spectrum vs isolate, and your personal comfort. Consider what you will actually tolerate on difficult days: oils are precise but taste can be strong, while water soluble options can mix into a drink. If you want help comparing formats, our CBD Buying Guide is a good starting point.
Can I use CBD with immunotherapy as well as chemotherapy?
Possibly, but you should treat this as a fresh question for your oncology team rather than assuming the answer is the same. Immunotherapy and chemotherapy can be used in different ways, and clinicians may be cautious about adding supplements that introduce extra variables. If your team approves CBD, keep your approach consistent and low dose, and ask what warning signs they want you to look out for.
Can CBD cause cancer?
People ask this because they are understandably cautious about anything new during treatment. In general, CBD sold as a food supplement in the UK is not positioned as something that causes or prevents cancer. The more realistic safety concern is product quality and contamination, plus whether CBD interacts with your medicines. If you are considering CBD, focus on transparent lab testing, avoid products making medical claims, and involve your oncology team so decisions are made with your full treatment plan in mind.
Is CBD ever helpful for nerve discomfort during chemo?
Some people explore CBD as part of a wider comfort routine when they are dealing with general aches or nerve-type sensations, but it is not a substitute for medical assessment. Chemo-related nerve symptoms can sometimes need prompt attention, dose adjustments, or specific supportive medicines. If you notice tingling, numbness, burning sensations, or changes in grip or balance, raise it with your team first. If CBD is approved, treat it as optional support, keep doses low, and track whether it makes you more sleepy or light-headed.
Key Takeaways
- CBD and chemotherapy can be a complex mix because of potential medicine interactions and overlapping side effects.
- Your oncology team needs specifics: product type, spectrum, dose, timing, and your full medication list.
- If you get approval, start low, keep it consistent, and track your response for 1 to 2 weeks.
- Prioritise quality: third-party lab reports and clear labelling matter more during treatment.
- If anything worsens, stop and get advice rather than trying to “push through”.
Conclusion
If you are wondering “can I use CBD with chemotherapy?”, you are not being difficult or overly cautious. You are being sensible. CBD may fit into some people’s wellbeing routines, but chemotherapy changes the risk equation. The two big priorities are interaction safety and product quality, and both require a conversation with your oncology team, not guesswork.
If you do get the green light, keep your approach steady: low dose, one product at a time, consistent timing, and a simple log of how you feel. Choose a format you can tolerate on your harder days, and avoid any brand making bold medical promises. CBD should support your routine, not add stress or uncertainty.
If you want a second pair of eyes on product labels or dosing basics, speak to Nick for free, practical guidance.